Tinea versicolor
OVERVIEW
What is tinea versicolor?
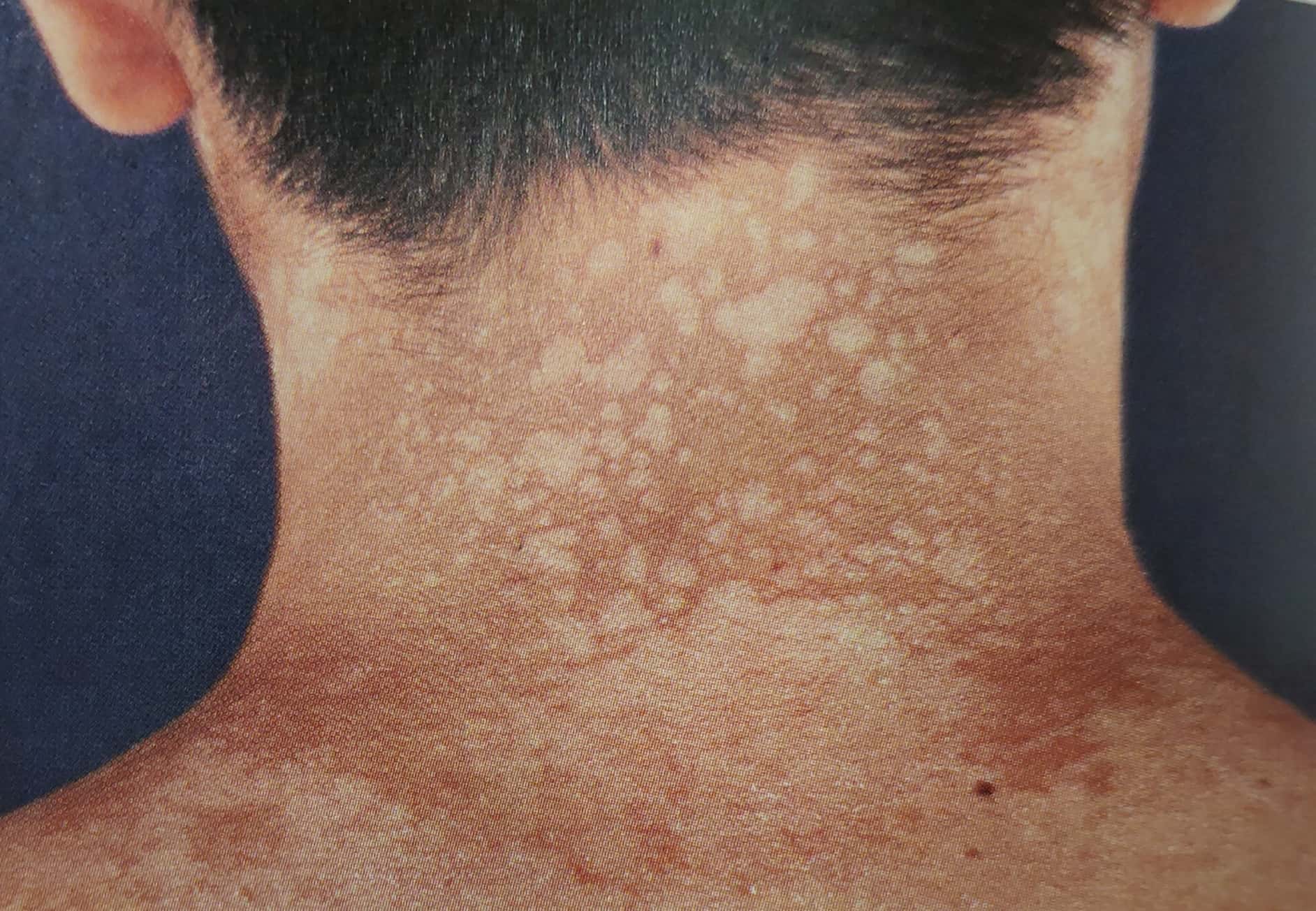
Tinea versicolor, also known as pityriasis versicolor or sweat spots, is a skin disease caused by Malassezia (a common fungus).
It often appears as scattered brown, red, or white patches on the trunk or upper limbs, with or without itching.
Treatment includes topical and oral antifungal medications. It is prone to recurrence, difficult to cure, and can negatively impact patients' lives and mental well-being.
Is tinea versicolor common?
This condition is very common, especially in summer.
Since predisposing factors include humid and stuffy environments, excessive sweating, etc., more cases are seen in summer.
SYMPTOMS
What are the common manifestations of tinea versicolor?
Tinea versicolor often appears as scattered brown, red, or white patches on the trunk or upper limbs, with fine scales on the rash surface. Patients usually have no obvious symptoms, but some may experience itching.
What serious consequences can tinea versicolor cause?
-
Tinea versicolor commonly occurs on the trunk and upper limbs. Many patients experience pigmentary changes after treatment, which can persist for months and significantly affect appearance.
-
Without active treatment, the rash may gradually expand and increase, potentially spreading to the entire chest and back.
-
Tinea versicolor tends to recur frequently, causing certain impacts on daily life and mental well-being.
CAUSES
What causes tinea versicolor?
Tinea versicolor is caused by the superficial fungus Malassezia.
Malassezia is normally part of the skin's microbial flora. When it transforms into a pathogenic hyphal form, it can lead to skin conditions, including tinea versicolor.
Who is more likely to develop tinea versicolor?
-
People who sweat excessively, have oily skin, or frequently stay in hot and humid environments are more prone to this condition.
-
Those with weakened immunity—such as individuals with malnutrition, diabetes, tumors, or those taking long-term immunosuppressants—are also more susceptible to tinea versicolor.
-
Additionally, studies suggest a genetic predisposition, meaning some people may develop tinea versicolor even without the above risk factors.
Is tinea versicolor contagious?
Although tinea versicolor is caused by a fungal infection, it is not contagious.
This is because the causative fungus, Malassezia, is part of the normal skin flora and present on everyone. It only becomes pathogenic—transforming into hyphae—under conditions like excessive heat, humidity, sweating, or low immunity. Even if a healthy person comes into contact with Malassezia from an affected individual, they will not develop the condition.
Is tinea versicolor hereditary?
Tinea versicolor is not hereditary but has a genetic predisposition. If a family member has tinea versicolor, other relatives may have a higher risk of developing it compared to the general population.
DIAGNOSIS
How is tinea versicolor diagnosed?
-
An experienced dermatologist can make a diagnosis after observing the rash.
-
For atypical cases, fungal microscopy and Wood's lamp examination can assist in diagnosing tinea versicolor.
Why are fungal microscopy and Wood's lamp examination performed for tinea versicolor? What precautions should be taken?
To diagnose tinea versicolor, doctors may perform fungal microscopy and Wood's lamp examination.
-
Fungal microscopy: Scales from the affected area are scraped for examination, which is non-invasive and painless. The doctor can directly observe Malassezia fungi under a microscope, with results available in about 20 minutes. To improve accuracy, avoid topical medications, especially antifungal drugs, for at least 3–5 days before the test. A positive result usually confirms tinea versicolor.
-
Wood's lamp examination: Under Wood's lamp, tinea versicolor lesions show yellow to yellow-green fluorescence. This test is also non-invasive, painless, and provides results within minutes.
Which diseases is tinea versicolor easily confused with? How to differentiate them?
Tinea versicolor is often confused with the following conditions:
-
Vitiligo: Vitiligo presents as completely depigmented patches, appearing whiter, and can occur anywhere on the body. Fungal tests are negative, and Wood's lamp shows porcelain-white fluorescence.
-
Pityriasis rosea: Pityriasis rosea typically manifests as multiple rose-colored patches on the trunk with fine, collarette-like scales. Fungal tests are negative.
TREATMENT
Which department should I visit for tinea versicolor?
Dermatology.
Is tinea versicolor treatment necessary? Can it heal on its own?
Tinea versicolor requires treatment. Without active treatment or incorrect treatment, the condition may worsen and persist for a long time.
How is tinea versicolor treated?
-
The most common and simplest method is topical antifungal medications, such as terbinafine, bifonazole, or ketoconazole ointments. Choose one and apply it twice daily for at least two weeks. Antifungal washes like ketoconazole or selenium sulfide can also be used during showers.
-
For patients with widespread or stubborn rashes, oral antifungal medications like itraconazole may be prescribed (typically 0.2 g daily for five days). However, this should only be used after evaluation by a dermatologist to avoid self-medication.
What are the common adverse reactions to tinea versicolor medications?
Topical treatments for tinea versicolor are generally safe, with most people experiencing no significant side effects. However, a few may develop allergic reactions like burning or redness.
Oral medications may have more side effects:
-
Possible gastrointestinal irritation, including nausea or loss of appetite.
-
Potential impact on liver and kidney function, requiring caution in patients with liver or kidney disease.
-
Risk of allergic reactions.
-
Possible interactions with other oral medications.
Therefore, oral treatment should only be used under professional medical guidance.
Can tinea versicolor cause other diseases?
After treatment, patients may still experience pigmentary changes, which may take months to gradually fade.
Can tinea versicolor be completely cured?
Since the triggering factors are difficult to eliminate, a complete cure is challenging, and recurrence rates are quite high.
DIET & LIFESTYLE
What should patients with tinea versicolor pay attention to in daily life?
In summer, the weather is hot and sweating is more frequent, so it is essential to prevent tinea versicolor recurrence:
- Maintain personal hygiene, especially skin cleanliness, and clean the skin promptly after sweating.
- Wash clothes promptly to ensure personal and environmental cleanliness.
- Focus on strengthening nutrition to improve the body's resistance.
- Treat other chronic conditions, such as diabetes, in a timely manner.
What dietary precautions should patients with tinea versicolor take?
Patients with tinea versicolor have no specific dietary restrictions; a healthy and balanced diet is sufficient.
-
When cooking, use less salt, less oil, and fewer high-sodium seasonings. Avoid pickled vegetables, cured meats, etc.
-
Avoid relying solely on refined grains like white rice and flour. Replace some staples with whole grains, legumes, potatoes, or pumpkin.
-
Balance meat and vegetables. Prefer white meats like chicken, duck, and fish, and limit fatty meats. Eggs and milk are important sources of protein and other nutrients.
-
For vegetarians, consume more beans and bean products to supplement protein.
-
Eat plenty of fresh fruits and vegetables.
-
Quit smoking and minimize alcohol consumption.
PREVENTION
How to prevent the recurrence of tinea versicolor?
Maintaining personal hygiene, regularly bathing with zinc pyrithione soap, or using topical antifungal medication once a month for preventive treatment can reduce the risk of tinea versicolor recurrence.
